How many people die from extreme temperatures, and how this could change in the future: Part one
Cold deaths vastly outnumber heat-related ones, but mostly due to “moderate” rather than extremely cold conditions.
Think about someone dying from extreme temperatures. You probably pictured someone passing out from heat stroke or dying from hypothermia.
But this is not how most people die from “heat”. They die from conditions such as cardiovascular or kidney disease, respiratory infections, or diabetes.1
Almost no one has “heat” or “cold” written on their death certificate, but sub-optimal temperatures lead to a large number of premature deaths. As we’ll see later, researchers estimate that it kills several million every year.
Older populations are usually most vulnerable to extreme temperatures. Most deaths occur in people older than 65. It’s important to consider what "death" means here and how deaths from extreme temperatures might compare to other causes. Being too hot or cold can increase our risk of developing certain health conditions or worsen existing ones. It can thereby lead to an earlier death than would have occurred if the temperatures were “optimal”.
How much time do hot or cold conditions take off someone’s life? It’s difficult to give precise estimates. One method that researchers often use is to look at excess death rates — which measure how many more people die in a given year compared to an “average” year — in a particularly warm or cold year. Looking at patterns of excess deaths gives some indication of whether temperature-related deaths were “brought forward” significantly or not.
A study by Nirandeep Rehill and colleagues examined death patterns in the United Kingdom over 50 years.2 It found that most cold-related deaths were among people who would not have died in the next 6 months. A later study looked at the impacts of high and low temperatures across a much larger sample of countries.3 It found that most temperature-related deaths reduced lifespans for at least one year. Most people died at least one year earlier, although there would be some that did lose less than this.
In this article, I will examine how many people die from heat and cold each year and how researchers estimate these numbers. In a follow-up article, I’ll look at how these risks could change in the future due to climate change.
A quick note on terminology: I will use the term “temperature-related deaths” from this point forward to refer to the combination of deaths from heat and cold conditions. When I use the term “heat”, I mean warm or hot.
Finding the “Goldilocks” spot where temperatures are most comfortable and healthy
To estimate temperature-related deaths, researchers estimate what is called the temperature-mortality relationship. This tells us how our risk of dying differs across the range of possible temperatures. To develop this relationship, scientists use real mortality records to understand “excess mortality” – how many “extra” deaths occur above a given expected baseline – at different temperatures. Plot this increased risk against temperature, and you’ll find a U-shaped curve.
Let’s look at these “mortality-temperature” curves. I’ve drawn a schematic below.
Your risk is lowest at the “optimal temperature” or “minimum mortality temperature”. This is the “Goldilocks” spot where the temperature is optimal: not too hot, not too cold, just right.
On either side of this optimum, your health risks increase. The shape of this curve matters. In most locations, the rise in risk is relatively low at ‘moderately cold’ temperatures before rising sharply in extremely cold conditions. And they have a steep rise in risk at very warm temperatures.
Let’s look at some real curves researchers use to estimate temperature-related deaths. Here, I’ve taken some of the curves used in a recent paper published in Nature Communications by Kai Chen and colleagues published in 2024.4 These curves are very similar to those used in other leading studies in this field.
I’ve picked a selection of cities from across the world.
What’s immediately obvious is how different these curves are.
First, they all have different optimal temperatures. It’s lower in cities in colder regions of the world: around 18°C in Vancouver and London, compared to 25°C in Buenos Aires and Beijing.5
Second, the shape of the curve varies a lot. In Paris, Vancouver, and Buenos Aires, mortality steepens at high temperatures. In Cape Town and Sao Paulo, it’s at colder temperatures. In some cities — such as Tokyo or Austin — risks are low across the temperature range.
These curves differ across places because people have acclimatized and adapted to the typical temperatures. This can be natural heat acclimatization — where our bodies physiologically adapt to tolerate hotter or colder temperatures — or technological adaptation, such as heating or air conditioning. People in Vancouver — and their homes — are well-adapted to very cold temperatures but are not adjusted to warm days.
Accordingly, mortality rates at very high temperatures can be low in Austin and Tokyo because most people have air conditioning. This is not true of Paris or London; it’s still rare across many European countries.
France was hit particularly badly when a large heatwave hit Europe in 2003. Around 15,000 people died. These temperatures — reaching as high as 40°C for more than a week in some cities — were an anomaly for the region in the early 2000s.6 But they would not have been noteworthy and not particularly lethal in other parts of the world. The problem was that local populations who experienced milder summers did not know how to react to extreme heat. Even simple adaptation measures such as rehydration would have saved some people’s lives.
This is important: with the right resources, humans have the ability to adapt to different temperatures. That matters for how we cope with a warming world.
Most people die from “moderately cold” conditions
If you look at many of the “optimal temperature” curves above, you’ll find that most of us spend most of the year a bit below the optimum. We most frequently experience temperatures a bit colder than is “best”.
This means most temperature-related deaths happen in “moderately cold” conditions, not on extremely cold or hot days. It’s not because the mortality risk in this zone is the highest, but the amount of time spent there is.
Again, this is not what most of us would think of as “cold conditions”. In the UK, this would include the increased risk of dying on days with a temperature of 10°C or 15°C. For us in Scotland, that’s not cold: that’s what we would consider a “nice summer’s day”.
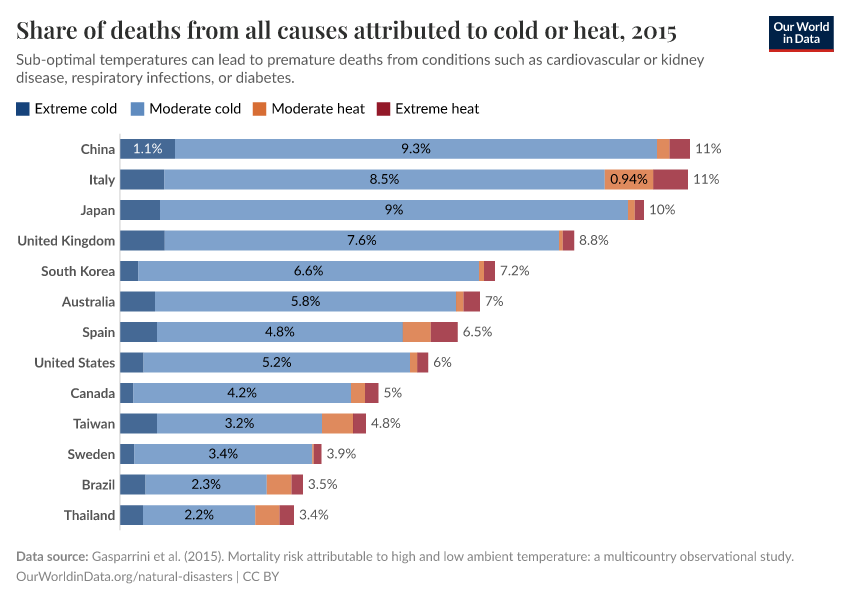
This situation is not unique to the UK: moderate cold dominates temperature-related deaths across most of the world. The chart below comes from a study by Antonio Gasparrini and colleagues, published in The Lancet.7 It estimates the share of deaths in each country that can be attributed to temperature but is broken down by moderate and extreme cold and heat. You can see that “moderate cold” dominates everywhere: from the UK and US to Thailand and Brazil.
How many people die from sub-optimal temperatures?
There are now a range of studies looking at this question. All tend to fall within the range of several million. Most of these deaths occur in elderly populations, and as I mentioned earlier, the amount of life lost in most cases is around 6 months to a few years.
A large global study by Qu Zaho and colleagues estimated temperature-related deaths from 2000 to 2019.8 They estimated that 5 million people die prematurely from cold or heat-related deaths each year. That was equal to 9.4% of deaths from all causes. Almost one in ten deaths.
An earlier study by Antonio Gasparrini and colleagues estimated that 7.7% of deaths in selected countries were attributed to temperature. This can’t be directly compared to the 9.4% above, nor can it be used to estimate a global figure because not all countries were included. But it does show that a significant fraction of deaths across Australia, Brazil, Canada, China, Italy, Japan, South Korea, Spain, Sweden, Taiwan, Thailand, the UK, and the United States are linked to sub-optimal temperatures.9
The Global Burden of Disease (GBD) study produces a lower death toll: its latest report attributed 1.9 million deaths to non-optimal temperatures in 2021. Other studies have suggested that this is probably underestimated due to differences in methodology and the inclusion of data from a smaller subset of countries.
Some researchers expect that as many as 1.8 million deaths each year are attributed to short-term temperature variability alone.10 Large swings from cold to warm conditions, or vice versa, can put pressure on our organ systems and increase health risks.
While estimates vary, depending on methodological differences, data quality, and assumptions about how humans respond to changes in temperature, the numbers are not small — they range from 1.7 to 5 million.
To take account of the age of people dying — and how much earlier they died — we would need to look at how many years of life had been lost. This multiplies the number of deaths by the number of years that their life was cut short. Unfortunately, only one of the studies above — the Global Burden of Disease — estimates the “Years of Life Lost” from sub-optimal temperatures. In estimates this was equal to 2% of the global total in 2021. That compares to 2.8% of deaths, which doesn’t have any weighting for age.
Cold-related deaths outnumber heat deaths in all countries
What’s consistent in these studies is that cold-related deaths vastly outnumber those from heat.
In the Global Burden of Disease study, cold-related deaths were around four times higher than heat-related ones.
The study that estimates that 7.7% of deaths were attributed to temperature found that 7.3% were from cold temperatures; 0.4% were from heat.
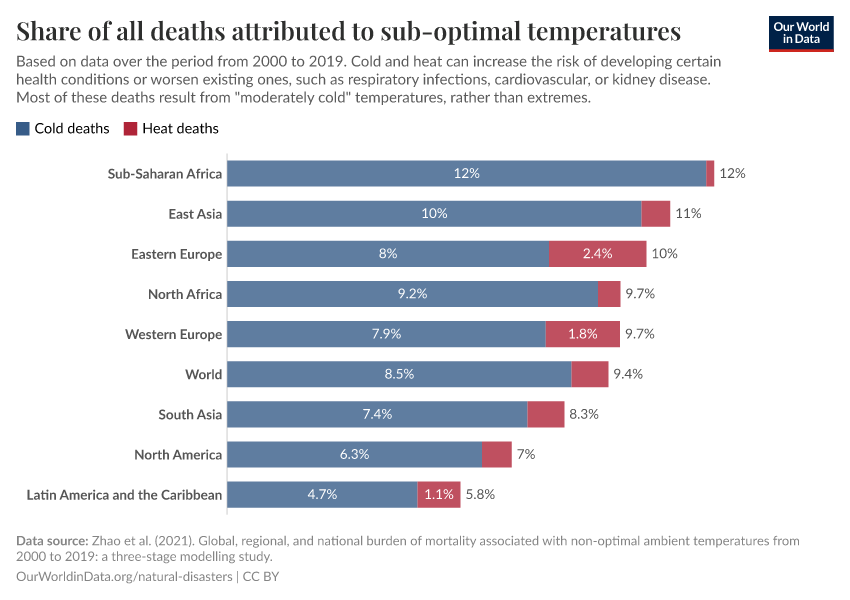
In the “5 million death” study, 9.4% of deaths were related to sub-optimal temperatures. 8.5% were cold-related, and 0.9% were heat-related. This skew was true across all regions.
You can see these results in the chart below.
Globally, cold deaths are 9 times higher than heat-related ones. In no region is this ratio less than 3, and in many, it’s over 10 times higher. Cold is more deadly than heat, even in the hottest parts of the world.
There is a long list of other studies that provide similar results. A study across 854 cities in Europe found that cold-related deaths were around ten times higher than heat-related ones.11 A detailed study across England and Wales found that cold-related deaths were two orders of magnitude higher.12 The same is true for China.13 And the United States.14
Again, to be clear, most of these deaths come from moderately cold conditions, not freezing temperatures. But it’s a robust and consistent result within the scientific literature: today, more people die from cold than heat.
This could change in the future as a result of climate change. In my next article, I’ll look at the increasing — and highly unequal — risk of heat deaths in a warming world.
Acknowledgements
Many thanks to Max Roser and Edouard Mathieu for their comments on this article and to Pierre Masselot for invaluable feedback on this research.
This article is part of a series on extreme heat:
How many people die from extreme temperatures, and how this could change in the future: Part one
Cold deaths vastly outnumber heat-related ones, but mostly due to “moderate” rather than extremely cold conditions.
How many people die from extreme temperatures, and how this could change in the future: Part two
Climate change will have very unequal impacts, with fewer deaths at higher latitudes but increased heatwave deaths across the tropics.
How can the world reduce deaths from extreme heat?
The world will need to adapt to increased temperatures. What can societies do to save lives?
Air conditioning causes around 3% of greenhouse gas emissions. How will this change in the future?
Demand is set to triple by 2050. Can it be met in an energy-efficient way?
Endnotes
Zhao, Q., Zhang, Y., Zhang, W., Li, S., Chen, G., Wu, Y., ... & Guo, Y. (2017). Ambient temperature and emergency department visits: Time-series analysis in 12 Chinese cities. Environmental pollution, 224, 310-316.
Lu, P., Zhao, Q., Xia, G., Xu, R., Hanna, L., Jiang, J., ... & Guo, Y. (2021). Temporal trends of the association between ambient temperature and cardiovascular mortality: a 17-year case-crossover study. Environmental Research Letters, 16(4), 045004.
Chen, R., Yin, P., Wang, L., Liu, C., Niu, Y., Wang, W., ... & Zhou, M. (2018). Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. Bmj, 363.
Benmarhnia, T., Deguen, S., Kaufman, J. S., & Smargiassi, A. (2015). Vulnerability to heat-related mortality: A systematic review, meta-analysis, and meta-regression analysis. Epidemiology, 26(6), 781-793.
Rehill, N., Armstrong, B., & Wilkinson, P. (2015). Clarifying life lost due to cold and heat: a new approach using annual time series. BMJ open, 5(4), e005640.
Armstrong, B., Bell, M. L., de Sousa Zanotti Stagliorio Coelho, M., Leon Guo, Y. L., Guo, Y., Goodman, P., ... & Gasparrini, A. (2017). Longer-term impact of high and low temperature on mortality: an international study to clarify length of mortality displacement. Environmental Health Perspectives.
Chen, K., De Schrijver, E., Sivaraj, S., Sera, F., Scovronick, N., Jiang, L., ... & Vicedo-Cabrera, A. M. (2024). Impact of population aging on future temperature-related mortality at different global warming levels. Nature Communications.
Yin, Q., Wang, J., Ren, Z., Li, J., & Guo, Y. (2019). Mapping the increased minimum mortality temperatures in the context of global climate change. Nature Communications.
Tobías, A., Hashizume, M., Honda, Y., Sera, F., Ng, C. F. S., Kim, Y., ... & Gasparrini, A. (2021). Geographical variations of the minimum mortality temperature at a global scale: a multicountry study. Environmental Epidemiology.
Due to further warming, summers are now approaching those conditions in 2003, but after a more gradual increase over the course of the 2010s.
Gasparrini, A., Guo, Y., Hashizume, M., Lavigne, E., Zanobetti, A., Schwartz, J., ... & Armstrong, B. (2015). Mortality risk attributable to high and low ambient temperature: a multicountry observational study. The Lancet.
Zhao, Q., Guo, Y., Ye, T., Gasparrini, A., Tong, S., Overcenco, A., ... & Li, S. (2021). Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. The Lancet Planetary Health, 5(7), e415-e425.
Gasparrini, A., Guo, Y., Hashizume, M., Lavigne, E., Zanobetti, A., Schwartz, J., ... & Armstrong, B. (2015). Mortality risk attributable to high and low ambient temperature: a multicountry observational study. The Lancet, 386(9991), 369-375.
Wu, Y., Li, S., Zhao, Q., Wen, B., Gasparrini, A., Tong, S., ... & Guo, Y. (2022). Global, regional, and national burden of mortality associated with short-term temperature variability from 2000–19: a three-stage modelling study. The Lancet Planetary Health, 6(5), e410-e421.
Masselot, P., Mistry, M., Vanoli, J., Schneider, R., Iungman, T., Garcia-Leon, D., ... & Aunan, K. (2023). Excess mortality attributed to heat and cold: a health impact assessment study in 854 cities in Europe. The Lancet Planetary Health, 7(4), e271-e281.
Gasparrini, A., Masselot, P., Scortichini, M., Schneider, R., Mistry, M. N., Sera, F., ... & Vicedo-Cabrera, A. M. (2022). Small-area assessment of temperature-related mortality risks in England and Wales: a case time series analysis. The Lancet Planetary Health.
Liu, J., Liu, T., Burkart, K. G., Wang, H., He, G., Hu, J., ... & Zhou, M. (2022). Mortality burden attributable to high and low ambient temperatures in China and its provinces: results from the Global Burden of Disease Study 2019. The Lancet Regional Health–Western Pacific.
Lee, J., & Dessler, A. E. (2023). Future Temperature‐Related Deaths in the US: The Impact of Climate Change, Demographics, and Adaptation. GeoHealth.
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this article, please also cite the underlying data sources. This article can be cited as:
Hannah Ritchie (2024) - “How many people die from extreme temperatures, and how this could change in the future: Part one” Published online at OurWorldinData.org. Retrieved from: 'https://ourworldindata.org/part-one-how-many-people-die-from-extreme-temperatures-and-how-could-this-change-in-the-future' [Online Resource]BibTeX citation
@article{owid-part-one-how-many-people-die-from-extreme-temperatures-and-how-could-this-change-in-the-future,
author = {Hannah Ritchie},
title = {How many people die from extreme temperatures, and how this could change in the future: Part one},
journal = {Our World in Data},
year = {2024},
note = {https://ourworldindata.org/part-one-how-many-people-die-from-extreme-temperatures-and-how-could-this-change-in-the-future}
}Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.